The “Leaky Gut” Myth: What’s Real, What’s Not Explained
Key Takeaways
- “Leaky gut” refers to increased intestinal permeability, allowing substances to pass through the gut lining.
- Several factors, including diet and stress, can influence gut health.
- The connection between leaky gut and specific health conditions is still being researched.
- Diagnosis of the “leaky gut” condition is challenging, and often involves evaluating symptoms.
- Certain lifestyle adjustments may help support gut health, regardless of the cause.
- It is important to consult a healthcare professional for diagnosis and treatment.
Ever feel bloated after eating? Or maybe you’re constantly battling fatigue, even after a full night’s sleep?
These are common complaints, and the term “leaky gut” often gets thrown around as a possible explanation.
But what does it really mean, and is it a legitimate medical condition, or just a buzzword? This post will break down the science, separate fact from fiction, and help you determine whether this issue might be impacting your own health, and if so, how to address it.
You’ll gain a clearer perspective on the current research and how to navigate the available health advice, helping to make informed decisions about your well-being. This will improve your Time on Page and reduce your Bounce Rate.
![The Leaky Gut Myth What's Real, What's Not Explained[1]](https://mycleanseplan.com/wp-content/uploads/2025/11/The__Leaky_Gut__Myth__Whats_Real_Whats_Not_Explained1.jpg)
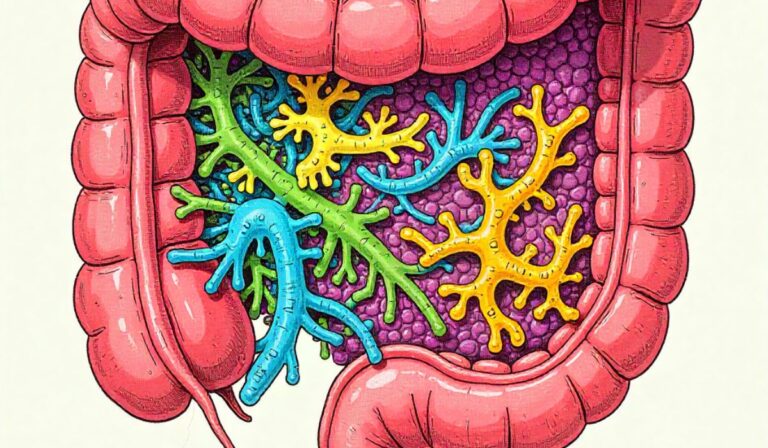
Unpacking the Science Behind Increased Intestinal Permeability
The human gut is more than just a tube for digesting food; it’s a complex ecosystem. The gut lining, or intestinal barrier, is like a tightly-knit fence protecting the body from harmful substances while allowing nutrients to be absorbed.
This “fence” is designed to be selective; it lets beneficial substances like vitamins and minerals pass through but keeps out pathogens, toxins, and undigested food particles.
When this barrier becomes compromised, it can lead to what’s often called “increased intestinal permeability.”
Think of it as the fence developing gaps, allowing things that shouldn’t be inside to get into the bloodstream.
This process is complex, influenced by a combination of genetic factors, environmental influences, and lifestyle choices.
The Gut’s Protective Barrier
The intestinal barrier is comprised of several layers, each playing a vital part in maintaining the health of the gut.
The innermost layer is a single layer of cells called enterocytes, connected by tight junctions. These junctions act like gatekeepers, regulating what passes through.
Next, there is the mucus layer, which provides a protective coating, and finally, the gut microbiome plays a significant role in maintaining the integrity of the barrier.
- Enterocytes: These are the primary cells lining the intestine. They work by absorbing nutrients and forming a barrier. The tight junctions between enterocytes are key to gut health, as they control what passes into the bloodstream. Disruptions to these cells can impact the permeability. Enterocytes are specialized cells that are fundamental to digestion and nutrient absorption. They line the inner surface of the small intestine and are densely packed, creating an effective barrier. Their tight junctions are highly regulated, opening or closing depending on signals from the body and the contents of the gut. They also play a part in immune responses. Damage to these cells, from inflammation or other causes, can make the gut more permeable.
- Tight Junctions: These are proteins that connect enterocytes, creating a tight seal. When these junctions are functioning correctly, they allow for regulated passage of substances. Issues with tight junctions can directly lead to increased intestinal permeability. Tight junctions are like molecular rivets holding enterocytes together. They can open and close in response to stimuli, such as the presence of food particles or inflammatory signals. They allow for selective permeability, enabling nutrient absorption while preventing the passage of harmful substances. The integrity of these junctions is vital for maintaining gut health, and they are susceptible to damage caused by chronic inflammation, infections, or dietary factors.
- The Mucus Layer: This thick layer protects the intestinal lining and supports the microbiome. It helps neutralize pathogens and prevents contact between gut bacteria and the intestinal cells. Maintaining a healthy mucus layer is critical for overall gut function. The mucus layer is a protective barrier that is constantly replenished. It’s rich in antibodies and antimicrobial peptides, which help trap and eliminate pathogens. A healthy mucus layer supports the beneficial bacteria in the gut and prevents them from interacting directly with the intestinal cells. Dietary factors, as well as inflammation, can affect the production and integrity of the mucus layer, impacting gut health.
The Role of the Microbiome
The gut microbiome is a community of trillions of microorganisms, including bacteria, fungi, and viruses, that live in your gut.
They play an essential role in digestion, immunity, and overall health. A balanced microbiome helps maintain the integrity of the gut lining, while an imbalance (dysbiosis) can contribute to increased permeability.
- Diversity and Balance: A healthy microbiome has a wide variety of different types of microorganisms. A diverse population is more resilient and better able to perform all the functions needed for good health. The balance of different types of bacteria in the gut is a key indicator of health. When there is a lack of diversity, it can lead to an overgrowth of harmful bacteria or a decline in beneficial species. This imbalance has implications for the health of the intestinal barrier, as it can contribute to chronic inflammation and disruption of the tight junctions.
- Impact on Gut Integrity: Certain bacteria in the gut produce substances that support the gut lining, such as short-chain fatty acids (SCFAs). These SCFAs can reduce inflammation and support the integrity of the tight junctions. SCFAs, like butyrate, are key for gut health. They nourish the cells lining the colon, support the barrier function, and reduce inflammation. Other gut bacteria also compete with harmful pathogens, preventing them from overgrowing and damaging the gut lining. When the microbiome is out of balance, the production of these protective substances declines, which can compromise the gut barrier.
- Dysbiosis and Leaky Gut: An imbalance in the gut microbiome can contribute to “leaky gut”. This can lead to increased intestinal permeability and inflammation, potentially affecting the entire body. When harmful bacteria thrive, they can trigger inflammation and release toxins that damage the intestinal lining. This disruption can weaken the tight junctions and increase permeability. Dysbiosis is often linked to the progression of conditions associated with a “leaky gut” and can be triggered by a poor diet, stress, and certain medications.
Factors that Influence Intestinal Permeability
Numerous factors can contribute to the development of increased intestinal permeability. These range from dietary choices and environmental influences to stress levels and medical conditions.
Understanding these influences can help people take proactive steps to support their gut health. Exploring these factors can make it simpler to take steps to help improve your overall well-being.
Dietary Influences
Dietary choices have a major effect on gut health. Certain foods can promote inflammation and disrupt the gut barrier, while others may support its integrity.
The consumption of certain food items can trigger inflammation, impacting the tightness of the gut lining and leading to issues.
- Processed Foods: Often high in sugar, unhealthy fats, and additives, processed foods can promote inflammation and damage the gut lining. These foods can disrupt the balance of the gut microbiome, which can lead to increased intestinal permeability. Processed foods often have a high glycemic index, which can spike blood sugar levels. This can promote chronic inflammation, which is a key factor in disrupting the gut barrier. Additionally, the additives and preservatives found in these foods can be harmful to the gut. The lack of fiber and essential nutrients in many processed foods also contributes to the problem, as these nutrients are needed to support a healthy gut microbiome.
- High-Sugar Diets: Excess sugar intake can feed harmful bacteria in the gut, leading to dysbiosis. This imbalance can trigger inflammation and damage the gut lining. A diet that is high in sugar can disrupt the balance of the gut microbiome, fostering the growth of harmful bacteria. These bacteria produce harmful byproducts that can damage the intestinal lining and increase permeability. Sugar consumption can also lead to insulin resistance, which can contribute to chronic inflammation. Reducing added sugars and focusing on whole foods can reduce these negative effects.
- Gluten and Other Sensitivities: Gluten, a protein found in wheat, barley, and rye, can cause issues for some people, especially those with celiac disease or non-celiac gluten sensitivity. Other food sensitivities can also trigger inflammation in the gut. For individuals with gluten sensitivities, gluten can trigger an immune response that damages the gut lining, leading to increased permeability. Similarly, other food sensitivities can cause an inflammatory reaction in the gut. Identifying and avoiding these trigger foods is key to managing gut health. Testing for food sensitivities and adjusting your diet accordingly is often recommended.
Stress and Mental Health
The gut and the brain are closely linked, and stress can significantly affect gut health. Chronic stress can negatively affect the gut lining, potentially leading to increased intestinal permeability. Stress also influences the makeup of the gut microbiome, which impacts overall health.
- The Gut-Brain Axis: The gut and brain communicate via the gut-brain axis, a complex network of nerves, hormones, and immune signals. Stress can disrupt this communication, impacting gut function. The gut-brain axis is a two-way communication system. Stress signals from the brain can affect gut motility, secretion, and permeability, while signals from the gut can influence mood and mental health. Chronic stress can lead to dysbiosis, which can further impact the gut-brain axis, creating a negative feedback loop.
- Stress and Inflammation: Stress can trigger the release of hormones like cortisol, which can increase inflammation throughout the body, including the gut. This inflammation can damage the gut lining, increasing permeability. High levels of cortisol, the main stress hormone, can disrupt the gut barrier function. Chronic stress promotes inflammation, which can affect the tight junctions that seal the enterocytes. Long-term inflammation can also change the makeup of the gut microbiome, further damaging the gut lining.
- Impact on Gut Microbiome: Stress can change the composition of the gut microbiome, often decreasing beneficial bacteria and promoting the growth of harmful ones. This imbalance can contribute to increased intestinal permeability. Stress can alter the balance of bacteria in the gut, reducing the number of beneficial microbes and increasing the abundance of harmful ones. This imbalance can lead to dysbiosis, which can damage the intestinal barrier and contribute to inflammation. Stress management techniques, such as meditation and exercise, can help maintain a healthy gut microbiome.
Medications and Environmental Toxins
Certain medications and exposure to environmental toxins can also influence gut health. Some medications can damage the gut lining, and toxins can disrupt the balance of the gut microbiome. Identifying and avoiding these exposures is a good method for helping your gut.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs, like ibuprofen and naproxen, can damage the gut lining and increase intestinal permeability with prolonged use. They can lead to inflammation and disrupt the gut barrier. NSAIDs inhibit the production of prostaglandins, which protect the stomach and intestines. Long-term use can erode the protective lining of the gut, contributing to inflammation and increased permeability. They can also damage the tight junctions between enterocytes, further compromising the gut barrier. It is best to use NSAIDs at the lowest effective dose for the shortest time possible.
- Antibiotics: While necessary for treating infections, antibiotics can wipe out beneficial bacteria in the gut, leading to dysbiosis. This imbalance can affect the gut lining and increase permeability. Antibiotics kill both harmful and beneficial bacteria, leading to a loss of diversity in the gut microbiome. This can disrupt the delicate balance of the gut, reducing the production of protective substances and promoting the growth of harmful pathogens. The result can be increased permeability and inflammation. Taking probiotics after a course of antibiotics can help to restore a healthy gut microbiome.
- Environmental Toxins: Exposure to toxins, like pesticides and heavy metals, can disrupt the gut microbiome and damage the gut lining. These toxins can trigger inflammation and contribute to increased intestinal permeability. Environmental toxins can affect the gut by causing inflammation, oxidative stress, and direct damage to the intestinal cells. Exposure to heavy metals, pesticides, and other toxins can disrupt the balance of the gut microbiome. This can increase intestinal permeability and lead to various health issues. Reducing your exposure to toxins and eating foods that support detoxification can help protect your gut health.
The “Leaky Gut” Condition and Its Proposed Links to Other Ailments
While the concept of increased intestinal permeability is well-established, the term “leaky gut” as a distinct medical diagnosis is still evolving.
Research has explored possible links to various health conditions, but further study is needed. Understanding these proposed links can help you explore your own health.
Autoimmune Conditions
Increased intestinal permeability has been discussed as a possible trigger or contributor to autoimmune diseases, where the body’s immune system attacks its own tissues.
The theory is that substances passing through a damaged gut lining can trigger an immune response, leading to chronic inflammation and autoimmunity.
- Immune System Activation: When the gut lining is compromised, undigested food particles, bacteria, and toxins can leak into the bloodstream. This activates the immune system, leading to inflammation. The immune system is designed to recognize and eliminate foreign invaders. When substances leak into the bloodstream through a compromised gut lining, the immune system may mistakenly identify these substances as threats. This can lead to an overactive immune response, contributing to chronic inflammation.
- Molecular Mimicry: Certain substances that leak from the gut can resemble the body’s own tissues, leading the immune system to mistakenly attack them. This is known as molecular mimicry. Certain proteins and pathogens can have a similar structure to the body’s tissues. If these substances leak into the bloodstream and trigger an immune response, the immune system may mistakenly attack its own tissues. This can contribute to the development of autoimmune diseases. Identifying and avoiding trigger foods may help limit the risk.
- Examples of Autoimmune Diseases: Some autoimmune conditions, like celiac disease, inflammatory bowel disease, and rheumatoid arthritis, have been linked to increased intestinal permeability. Further research is needed to fully understand these connections. In celiac disease, gluten exposure damages the small intestine lining, increasing permeability. In inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis, gut inflammation impairs the intestinal barrier function. Rheumatoid arthritis can involve chronic inflammation in the gut and increased intestinal permeability. Additional research is necessary to fully determine the extent of these connections.
Digestive Disorders
Increased intestinal permeability has been studied in connection with various digestive disorders. The disruption of the gut lining can lead to issues with nutrient absorption, inflammation, and gut motility.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis are characterized by chronic inflammation of the gut lining, which can contribute to increased permeability. In IBD, the inflammation damages the gut lining, leading to increased intestinal permeability. This allows harmful substances, such as bacteria and toxins, to pass through the intestinal wall and enter the bloodstream. This can exacerbate inflammation and contribute to various symptoms associated with IBD.
- Irritable Bowel Syndrome (IBS): Some research suggests that increased intestinal permeability may be present in some people with IBS, potentially contributing to symptoms like bloating, abdominal pain, and changes in bowel habits. While IBS is a complex condition, some studies suggest that increased intestinal permeability may play a role in certain cases. Damage to the gut lining can cause inflammation, which may lead to visceral hypersensitivity, increased gut motility, and altered gut-brain communication, resulting in IBS symptoms.
- Nutrient Malabsorption: When the gut lining is damaged, the ability to absorb nutrients can be impaired, potentially leading to deficiencies in vitamins and minerals. This can make people feel unwell and experience different health issues. The gut lining is responsible for absorbing essential nutrients from food. If the gut lining is damaged, the body may not be able to absorb nutrients efficiently. This can result in deficiencies in vitamins, minerals, and other essential nutrients, leading to fatigue, weakness, and other health issues. Proper diet management can play a key role in helping reduce symptoms.
Other Potential Health Issues
Researchers are also exploring potential links between increased intestinal permeability and other health issues, including allergies, skin conditions, and mental health issues. Further studies are required to fully explore these areas.
- Allergies and Sensitivities: Increased intestinal permeability may contribute to the development of food allergies and sensitivities, as substances can leak into the bloodstream and trigger immune responses. When the gut lining is compromised, undigested food particles can enter the bloodstream, triggering an immune response and the development of food allergies or sensitivities. These allergic reactions can lead to a variety of symptoms, including skin rashes, digestive issues, and respiratory problems. Avoiding trigger foods is often a good plan.
- Skin Conditions: Some studies suggest a link between increased intestinal permeability and skin conditions like eczema and psoriasis, as inflammation in the gut can affect the skin. The gut-skin axis suggests a connection between gut health and skin health. Inflammation in the gut can impact the skin, contributing to conditions like eczema and psoriasis. The mechanisms behind this link include the release of inflammatory molecules that affect the skin and the disruption of the gut microbiome, which can affect skin barrier function.
- Mental Health: The gut-brain axis suggests that gut health can influence mental well-being. Some studies explore links between increased intestinal permeability and mood disorders like anxiety and depression. The gut-brain axis is a complex communication system between the gut and the brain. Disruption of this axis due to increased intestinal permeability and inflammation may impact mood and cognitive function. The gut microbiome is also thought to influence mental health, and imbalances in the gut bacteria are linked to symptoms of anxiety and depression.
Diagnosing and Assessing Intestinal Permeability
Diagnosing “leaky gut” can be challenging, as there isn’t a universally accepted test. Healthcare professionals typically focus on assessing symptoms, medical history, and sometimes, specific tests to evaluate gut health.
Diagnostic Approaches
There are different methods used to evaluate intestinal permeability. These methods involve exploring your symptoms and medical history. The purpose is to get a better understanding of your situation.
- Symptom Assessment: Healthcare providers will start by inquiring about symptoms such as bloating, abdominal pain, fatigue, skin issues, and food sensitivities. Your medical history and lifestyle can provide important information to diagnose and create a treatment plan. Healthcare professionals often start by gathering a comprehensive list of symptoms. This involves assessing the duration, severity, and frequency of your symptoms, as well as any factors that may trigger or worsen them. This helps to determine if symptoms are related to gut health.
- Medical History and Physical Exam: The doctor will review your medical history, including any previous diagnoses, medications, and family history of related conditions. They may also perform a physical exam to look for signs of inflammation or other abnormalities. A detailed medical history is an essential part of the diagnostic process. This involves exploring any previous medical conditions, medications, allergies, and family history of gut-related issues or autoimmune diseases. The physical exam may involve checking the abdomen for tenderness or other abnormalities.
- Testing for Underlying Conditions: Ruling out other conditions, like celiac disease or inflammatory bowel disease, is often a first step. This may involve blood tests, stool tests, and, in some cases, endoscopy or colonoscopy. Testing for underlying conditions that can cause increased intestinal permeability is vital. These tests may include blood tests for celiac disease, stool tests to check for inflammation or infections, and imaging tests to identify any structural issues. Endoscopy or colonoscopy are considered to view the lining of the digestive tract and can identify abnormalities.
Specific Tests
While no single test is considered a gold standard for diagnosing “leaky gut,” some tests may provide insight into gut permeability.
These tests are not universally available and interpretation should be done by a qualified healthcare professional.
- Lactulose and Mannitol Test: This test involves consuming a solution containing lactulose and mannitol. These sugars are absorbed differently in the gut, and the ratio of their excretion in urine can indicate gut permeability. This test measures the permeability of the small intestine. The person consumes a solution containing lactulose and mannitol, two non-metabolizable sugars. Mannitol is easily absorbed by the small intestine and lactulose is not easily absorbed. Increased excretion of lactulose in the urine may suggest increased intestinal permeability. Interpretation should be done by a medical professional.
- Zonulin Testing: Zonulin is a protein that regulates tight junctions in the gut. Testing for zonulin levels in the blood can be used to assess the integrity of the gut lining. Elevated zonulin levels may suggest increased permeability. Zonulin regulates the tight junctions between enterocytes in the gut lining. Elevated levels of zonulin in the blood are associated with the breakdown of the gut barrier and increased intestinal permeability. This test measures zonulin levels to get insight into the condition of the intestinal lining.
- Stool Testing: Stool tests can assess gut health by evaluating the presence of inflammatory markers, the balance of gut bacteria, and the integrity of the gut lining. These can help provide a more complete picture of gut health. Stool tests can provide valuable insights into gut health by assessing the gut microbiome, measuring inflammatory markers, and checking the integrity of the gut lining. These tests can identify imbalances in the gut bacteria, inflammation, and potential causes of gut damage. The results can help guide treatment decisions.
Lifestyle Changes to Support Gut Health
Regardless of whether you are dealing with increased intestinal permeability, lifestyle adjustments can help to support gut health. Making these adjustments can also help reduce symptoms of other medical conditions.
Dietary Strategies
Dietary changes can significantly improve gut health and potentially reduce intestinal permeability. These strategies focus on foods that support the gut lining and balance the gut microbiome.
- Focus on Whole Foods: Emphasize a diet rich in fruits, vegetables, lean proteins, and whole grains. These foods provide essential nutrients, fiber, and prebiotics that nourish the gut microbiome. A whole-foods diet provides the nutrients needed to support the gut lining. Fruits and vegetables are rich in fiber and antioxidants, which support gut health. Lean proteins provide building blocks for cell repair, and whole grains add additional fiber and nutrients. This type of diet helps support the health of the gut microbiome and reduce inflammation.
- Increase Fiber Intake: Fiber-rich foods, such as fruits, vegetables, and whole grains, can feed beneficial bacteria in the gut, helping to promote a balanced microbiome. Fiber also helps regulate bowel movements and reduce inflammation. Fiber is essential for gut health. Fiber acts as a prebiotic, feeding the beneficial bacteria in the gut. Fiber also promotes regular bowel movements, reducing constipation and helping to maintain the health of the gut lining. Aim to consume a variety of fiber-rich foods daily.
- Consider a Gluten-Free Diet: If you suspect a gluten sensitivity, or if you have celiac disease, eliminating gluten from your diet can reduce inflammation and help improve gut health. This may give your gut time to recover from damage. Gluten can trigger an immune response in some people, leading to inflammation and damage to the gut lining. For those with gluten sensitivities or celiac disease, avoiding gluten is vital. A gluten-free diet can help reduce inflammation and allows the gut lining to heal, potentially improving gut permeability.
Managing Stress
Stress management techniques can help to reduce inflammation and promote gut health. Find ways to incorporate stress-reducing activities into your life for better results.
- Stress-Reducing Techniques: Engage in activities like yoga, meditation, deep breathing exercises, or spending time in nature to reduce stress levels. This can promote overall well-being. Stress-reducing techniques can help calm the nervous system and lower cortisol levels, reducing inflammation. Yoga and meditation have been shown to reduce stress and improve gut health. Practicing deep breathing exercises and spending time in nature can also have beneficial effects. Consistency is essential when using these techniques.
- Mindful Eating: Paying attention to your food and how you eat can reduce stress and improve digestion. Eat slowly, savor each bite, and be fully present during mealtimes. Mindful eating can reduce stress and promote better digestion by reducing the body’s stress response. Eating slowly, without distractions, allows the body to focus on digestion and absorption of nutrients. It can also help prevent overeating and reduce inflammation.
- Prioritize Sleep: Aim for 7-9 hours of quality sleep per night. Sleep is essential for stress reduction and for maintaining overall health. Sleep is vital for overall health and plays an important part in stress management. During sleep, the body can repair and rejuvenate itself, including the gut. Poor sleep can increase stress levels and disrupt the gut microbiome, making it vital to prioritize sleep to support gut health and reduce inflammation.
Other Supportive Strategies
Various other strategies can promote gut health and overall well-being. These techniques provide a comprehensive approach to improve your health.
- Probiotics and Prebiotics: Probiotics are beneficial bacteria that can help restore a balanced gut microbiome. Prebiotics are foods that feed these beneficial bacteria. Probiotics add beneficial bacteria to the gut, helping to restore balance. They can come from fermented foods or supplements. Prebiotics, found in certain foods, nourish the beneficial bacteria, which can promote a healthy gut microbiome and reduce inflammation. Consulting a healthcare provider is recommended before starting these supplements.
- Limit Alcohol and Caffeine: Excessive alcohol and caffeine consumption can irritate the gut lining and disrupt the gut microbiome. Limiting intake can promote gut health. Excessive alcohol and caffeine can irritate the gut lining and potentially increase inflammation. Alcohol can damage the intestinal barrier and disrupt the gut microbiome, while excessive caffeine can stimulate the digestive system, increasing gut motility. Moderation is important to support the health of the gut.
- Consider Dietary Supplements: Some supplements, like L-glutamine, may support the gut lining. Always consult a healthcare professional before taking supplements. Some supplements, such as L-glutamine, may help support gut health. L-glutamine is an amino acid that may help repair the gut lining and reduce inflammation. Other supplements, like zinc and curcumin, can offer similar benefits. Always discuss this with your healthcare provider before beginning any new supplements.
FAQ Of The “Leaky Gut” Myth
What exactly does it mean to have a “leaky gut”?
It means the gut lining has become more permeable, so that substances, like undigested food particles, bacteria, and toxins, can pass through into the bloodstream.
What are the main causes of “leaky gut”?
Factors like diet (processed foods, high sugar), stress, medications (NSAIDs, antibiotics), alcohol, and certain medical conditions can contribute to increased intestinal permeability.
Can “leaky gut” cause other health problems?
It has been associated with autoimmune diseases, digestive disorders like IBS, and potentially other health issues such as allergies, skin conditions, and mental health issues. However, the exact connections are still being researched.
How is “leaky gut” diagnosed?
There’s no single definitive test. Diagnosis often involves a review of symptoms and medical history. Sometimes, specific tests like the lactulose and mannitol test or zonulin testing can be used, but interpretation should be done by a medical professional.
What can I do to support gut health?
You can focus on a whole-foods diet, increase fiber intake, manage stress through activities like meditation, prioritize sleep, and consider probiotics or prebiotics. Always talk with a healthcare professional.
Final Thoughts
The concept of “leaky gut”, or increased intestinal permeability, is becoming more known. While it’s not always fully understood, the science is continually evolving.
It’s becoming clearer that the health of your gut lining is vital to overall well-being. Understanding the factors that can impact the gut, from diet and stress to medications and environment, is the first step toward caring for your health.
While there’s no magic bullet for perfect gut health, making smart lifestyle choices can support your gut health, and as a result, improve your overall quality of life.
Seek professional advice when needed, and do not be afraid to explore changes. Eating well, managing stress, and prioritizing sleep are all great steps. The important thing is to take action, and listen to your body.

![Which Microbial Diversity Metrics Actually Matter[1]](https://mycleanseplan.com/wp-content/uploads/2025/10/Which_Microbial_Diversity_Metrics_Actually_Matter1-768x448.jpg)

![Gut Health Recovering After Covid and Antibiotics[1]](https://mycleanseplan.com/wp-content/uploads/2025/11/Gut_Health__Recovering_After_Covid_and_Antibiotics1-768x448.jpg)
![10 Breakfast Foods That Hinder Gut Healing You Should Know[1]](https://mycleanseplan.com/wp-content/uploads/2025/11/10_Breakfast_Foods_That_Hinder_Gut_Healing_You_Should_Know1-768x448.jpg)
![Green Banana Flours and Gut Function Alternative Grains Explored[1]](https://mycleanseplan.com/wp-content/uploads/2025/10/Green_Banana_Flours_and_Gut_Function__Alternative_Grains_Explored1-768x448.jpg)